

During Paris Roubaix Femmes avec Zwift Ellen van Dijk proved the world that it is absolutely possible for elite cyclist to have a great comeback in the saddle after a pregnancy. Her teammate Lizzie Deignan proved this 2 years ago already when she won the race, but the performance of Van Dijk understated this. However, it is not a given and some caution is needed.
The journey of elite cyclists through pregnancy and the postpartum period is an evolving narrative, marked by resilience, determination, and a quest for balance between athletic excellence and motherhood. As notable figures in the sports world demonstrate, motherhood need not signal the end of a flourishing athletic career; instead, it becomes a testament to the enduring spirit of female athletes and an inspiration for women and girls worldwide. However, behind the scenes lies a complex tapestry of challenges, uncertainties, and uncharted territories that demand attention and understanding. In this article, we delve into the multifaceted dynamics of pregnancy, postpartum recovery, and return to sport in the women’s cycling, drawing insights from a synthesis of research findings, athlete experiences, and emerging guidelines.
During pregnancy, many women cyclists may wonder whether they can continue riding. The answer often depends on individual circumstances, including the mother’s health, the stage of pregnancy, and previous cycling experience. While some women comfortably cycle throughout their pregnancies, others may need to modify their routines or discontinue cycling temporarily under medical advice.
Recent studies have shed light on the physiological adaptations and performance changes experienced by pregnant cyclists. One such study found that despite structured endurance training and increases in red blood cell volume and blood volume, there was no increase in absolute VO2peak from gestational week 2 to 14. However, power output at specific lactate levels was maintained until later gestational weeks. After delivery, there was a quick improvement in endurance performance when gradually returning to pre-pregnancy training levels, illustrating a disassociation between haematological values and VO2peak during pregnancy.
The effects of high-intensity interval training (HIIT) on pregnant women had been demonstrated as safe and potentially beneficial. Using real-time fetal heart rate monitoring during high-intensity exercise was found no adverse effects on fetal well-being. Additionally, significant decreases in umbilical artery Doppler indices post-exercise suggest improved fetal perfusion, highlighting the potential benefits of HIIT during pregnancy.
The most recent physical activity and exercise in pregnancy guidelines represent a paradigm shift, emphasizing the importance of exercise in optimizing maternal and fetal health. While further research on HIIT during pregnancy is warranted, its potential as a time-efficient and enjoyable exercise option for expectant mothers is promising.
There is little scientific evidence on the risks of resistance training during pregnancy. In general, it is advised that athletes pay attention to technique and safety. Caution is recommended when weightlifting on the back due to the concerns related to vena cava compression.
Medical screening during pregnancy and additional testing and follow-up
In the absence of maternal or fetal contraindications, exercise prescription in pregnancy includes the same principles and elements used for the general non-pregnant population, with the distinction that pregnancy is associated with significant anatomical, hormonal, metabolic, cardiovascular and pulmonary changes/adaptations.
Screening for high level exercisers and elite athletes, a thorough clinical evaluation should be conducted to ascertain that there are no medical or obstetrical reasons to either avoid exercise completely, or to modify exercise routines. Absolute contraindications, relative contraindications and warning signs specific to elite athlete athletes exercising in pregnancy have been adapted from the American College of Obstetricians and Gynecologists (ACOG) guidelines. As pregnancy progresses, new conditions may arise and risk stratification may change from no contraindications, to relative contraindications, to absolute contraindications and athletes and their coaches need to respond accordingly. Given, the lack of research available to counsel elite athletes who choose to exercise above moderate levels, particular attention should be given to fetal growth in the second and third trimester.
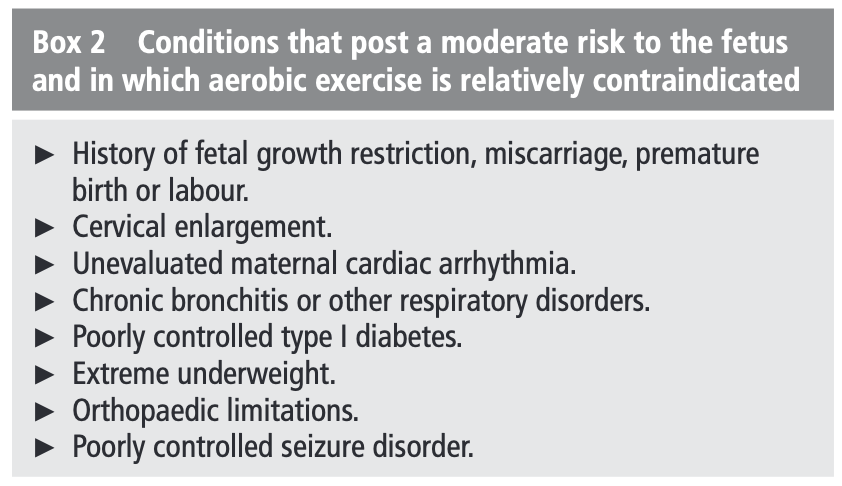
Absolute and relative contraindication to aerobic exercise during pregnancy
Women without contraindications are recommended to exercise regularly during pregnancy while being regularly reassessed. While engaging in exercise during pregnancy, the following may serve as warning signs to stop exercising: vaginal bleeding, regular painful contractions, amniotic fluid leakage, dyspnoea prior to exertion, dizziness/syncope, headache, chest pain, muscle weakness, calf pain or swelling.
Physicians, midwives, physiotherapists and coaches looking for resources to evaluate elite pregnant athletes’ risk for exercising in pregnancy are referred to the Physical Activity Readiness Medical Examination (ParMed-X) for Pregnancy, a guideline for health screening prior to participation in a prenatal fitness class or other exercise.
Advice on Some General Concerns Related to Exercise:
– Hyperthermia: Raising body core temperature above 39°C due to infection, in the first days of pregnancy may increase the risk of fetal neural tube defect abnormalities. The risk is highest 20–30 days after conception. Hyperthermia should be avoided especially during the first trimester. Exercise at 60%–70% of VO2max does not raise core temperature above 38°C. Moderate exercise during gestation will not raise body core temperature above this threshold. Thermoregulation steadily improves during pregnancy, as reflected by a gradual decline in rectal temperature.
– Supine position: There have been few studies evaluating the maternal and fetal effect of exercising in the supine position, although caution is recommended in many guidelines due to the potential risk of decreased venous return and decreased uterine blood flow. Orthostatic hypotension may occur from supine position and standing motionless. Should side effects, such as dizziness, occur while engaging in such activities, they should be discontinued. Side effects are more likely to occur after 28 weeks gestation. To reduce potential risks, exercises normally done in the supine position may be modified by tilting the torso to 45 degrees or doing the exercises in side-lying, sitting or standing positions. Some studies report no adverse effect with exercise in the supine position for 2–3min at a time.
– Altitude: A special case concerns low-land athletes who want to train at high altitude, since both hypoxia and exercise decrease blood flow to the uterus, and their combination leads to a decrease in arterial oxygen saturation, it seems advisable to refrain from high-intensity training regimens at altitudes >1500–2000m during pregnancy for those not acclimatized.
– Nutrition: Pregnant women are advised to follow their country-specific recommendations and seek advice from their antenatal care providers regarding nutrient supplementation before and during pregnancy. Pregnant elite athletes should also pay special attention to adequate energy intake to achieve recommended gestational weight gain.
– High-Intensity Endurance Training and Testing of VO2max: Like recommended for pregnant women in the general population, pregnant elite athletes may use perception of exertion or fatigue to gauge their training intensity. Pregnant elite athletes who have access to more sophisticated evaluation are recommended to refrain from training at intensities >90% of their VO2max, although there has not yet been research in pregnant athletes whose baseline VO2max is already significantly higher than the general population.
Return to play post partum
As van Dijk and Deignan proved, athletes strongly emphasized the need for flexible return-to-sport timelines that would allow them to resume training on their own terms, without penalizing their success as athletes. Fear of losing their position on a team or not being able to qualify for major competitions drove many athletes to return to sport too soon, resulting in injuries.
The 2016 International Olympic Commettee guidelines likened vaginal birth to an acute sports injury and advocated for increased research to develop return-to-sport protocols for the postpartum period.
Currently, there are few evidence-informed recommendations for postpartum return to sport, often relying heavily on medical clearance at the 6-week postpartum checkup before resuming activity, with limited guidance thereafter. In 2019, a group of physiotherapists developed return-to-running guidelines for the postpartum period, presenting the first evidence-based framework for health professionals. These guidelines highlighted the need to achieve specific milestones before resuming high-impact/intensity exercise and provided key considerations for common postpartum complaints, including musculoskeletal pain and urinary incontinence.
The timing and success of returning to elite sport post-pregnancy have been highly variable and complicated, as athletes have had to balance their mental health with high volumes of training and breastfeeding.
To further complicate their experiences, athletes have had to navigate their own return with a severe lack of evidence-based return-to-sport protocols. Previous research has documented the critical need for organizational and sponsorship support for elite athlete mothers. Similarly, athletes in our study strongly emphasized the critical role that sporting organizations and coaches play in supporting postpartum athletes. For example, some professional organizations, such as the Professional Triathlon Organization and Ladies Professional Golf Association, have recently developed parental leave policies supporting childcare and maternity leave. In 2018, the Women’s Tennis Association implemented seeding policies to ensure that postpartum athletes would not be penalized. Formal protections to support mother-athletes are emerging at the professional level but remain elusive in most other organizations.
After childbirth, female cyclists often eagerly anticipate resuming their favorite activity. However, the process of returning to cycling requires patience, careful planning, and consideration of the body’s recovery needs.
The progressive and challenging transition from athlete to athlete-mother has been described previously in the literature. Although this dual identity can be complementary, it is often fraught with social, cultural, and financial challenges.
Athletes highlighted both the challenges and joys of motherhood but also identified key strategies that sporting organizations, coaches, and athletes themselves can adopt to reduce these barriers and facilitate the retention of mothers in elite sport. Athletes emphasized the urgent need to develop policies that do not penalize them for taking parental leave. They called for clear policies on the duration and amount of funding, how pregnancy and parental leave would impact their eligibility and ranking in future competitions, as well as policies and individualized planning for return to training to support athlete well-being. Although the need for formal information sources during pregnancy has been previously recognized, postpartum athletes identified the lack of evidence-based information guiding return to sport, as well as awareness about the necessity for lactation, pelvic floor health, and mental health services specializing in working with elite athletes.
The journey from elite athlete to athlete-mother represents a paradigm shift, challenging traditional notions of athletic performance and motherhood. As we reflect on the stories of resilience, perseverance, and adaptation shared by elite cyclists, it becomes evident that motherhood is not a hindrance but rather a catalyst for transformation. Yet, amidst the triumphs lie poignant reminders of the need for greater support, resources, and understanding for athlete mothers. Moving forward, it is imperative for sporting organizations, coaches, and policymakers to heed the voices of these athletes, implementing policies and initiatives that foster inclusivity, flexibility, and empowerment. By embracing the unique intersection of athleticism and motherhood, women’s cycling can chart a course towards a future where every athlete has the opportunity to thrive, both on and off the saddle.